
The history is usually fairly similar to buckle fractures there is usually a fall on outstretched hand followed by pain and swelling. (Editors note:In fact Emily did just this: she took her two young nephews romping in the woods and bent a lot of sticks, all in the name of medical science.) Again, like the torus fracture, this is the result of the softer bones of children. This is what happens in paediatric greenstick fractures: they are partial fractures where the cortex is broken on only one side of the bone. Imagine walking in the woods, picking up a stick and bending it* the tough bark on one side will break but the bark on the other side remains intact. Greenstick fractures are unique to paediatrics, usually only seen in children under 10 years old. Watch this space for results, it could be interesting. The team are looking at pain, functional improvement and complications. Children with distal radius buckle fractures are being randomised to either management with a soft bandage or rigid immobilisation (splint or casting, depending on current practice of the treatment centre). This question is currently being addressed by the FORCE trial. Add to this the growing acceptance that splints may not actually improve pain control or affect complication rates and the question starts to emerge: do we actually need to immobilise these fractures? Although a removable splint possibly ensures maximal comfort with a theoretical advantage of minimising refracture, the flip side is that function is restricted. However, they should avoid sport for the first 3 weeks and no contact or team sport for a total of 6 weeks.īut, the question has been raised as to whether we actually need to immobilise these types of fractures at all.

Patients may report some stiffness of the wrist when the splint comes off but they shouldn’t need formal physiotherapy.īuckle fractures have a risk of refracture so it is important to counsel patients about return to sport and usual activities: once discharged from ED these children can go back to school and can partake in usual play.

Many centres follow-up in virtual fracture clinics some don’t follow-up at all as risk of complications is so low. These fractures will heal with minimal or no complications and do not require follow up in a face-to-face trauma or fracture clinic. The splint should be worn for 3 weeks, but can be removed or earlier if the child is pain free. In really young children, if there is no splint small enough they will be put in a plaster cast. Treatment of buckle fractures: the controversyīuckle fractures are treated with analgesia, rest and support.Īt the moment there is a degree of international (and national) variation in what people do for “support” so do check your local policy, but current evidence suggests immobilising with a removable splint will result in excellent healing. For those familiar with the Greek columns, outside BMA House and the Royal College of Surgeons in London, the bulgy bit at the top or bottom of the straight column is known as the “torus” of the column. To me, the name “buckle fracture” is very descriptive and visual, so I favour it over “ torus fracture”…until I found out that “torus” is the Greek for “ bulge” (ish).

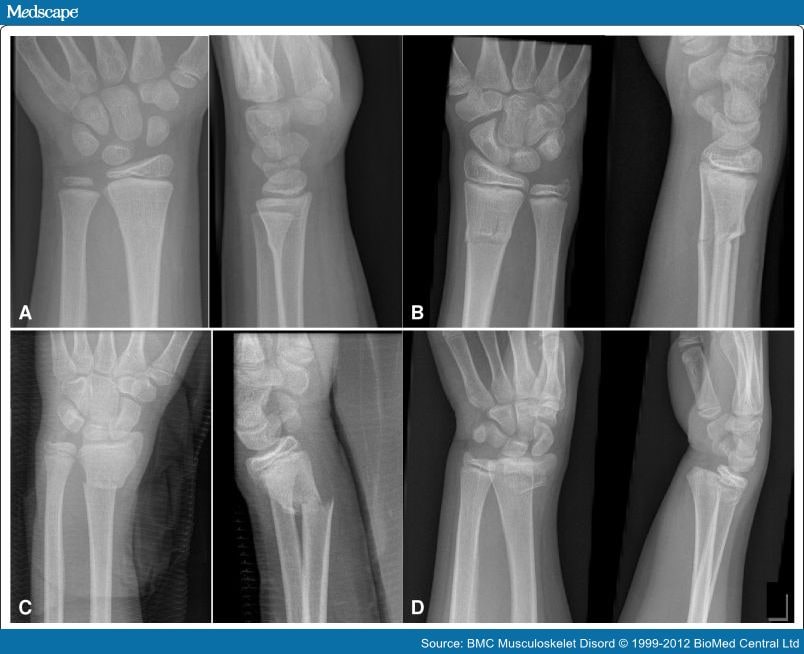
This buckling of the bone happens because the paediatric bone is soft. Much like when the front of a car drives into a lamp post, the front of the car will crumple. Torus fractures are very stable fractures as the cortex crumples and buckles rather than snaps in two. They are caused by a longitudinal force through a long bone, usually from a Fall on to an Outstretched Hand ( FOOSH). They are a common fracture of the distal radius +/- ulna where only one side of the bone buckles but the other side of the bone is unaffected. Torus fractures can, in theory, occur in any soft, compressible bone, but the term “ torus fracture” is most frequently used in the context of radius or ulna fractures. Torus fractures and buckle fractures are the same thing and the terms can be used interchangeably. But that just isn’t true while they have things in common, they also have significant differences. Which means you will often hear people say “ they are the same thing” (in fact, if you google “buckle fractures” they often offer up beautiful examples of…greenstick fractures!). They are both almost exclusively seen in children due to the cartilaginous, compressible, soft nature of young bones. They are often discussed alongside each other as they have several things in common. Wrist and forearm fractures account for half of all paediatric fractures. Forearm fractures (torus and greenstick fractures combined) are very common in children and happen in about 1 in 100 children.


 0 kommentar(er)
0 kommentar(er)
